The National Comprehensive Cancer Network (NCCN) was created in 1995 as a national alliance to develop and institute standards of care for the treatment of cancer and to perform outcomes research. They are the recognized standard for clinical policy in oncology and are the most comprehensive and most frequently updated clinical practice guidelines available in any area of medicine. These guidelines apply to 97% of all cancers affecting patients, and are updated on a continual basis. The guidelines are developed through a review of evidence integrated with expert medical judgment and recommendations by panels that are made up of representatives from the 28 NCCN Member Institutions.
NCCN Treatment Standards for CRC (Version 2.2020 – March 3, 2020)
In patients with a pedunculated or sessile polyp, the NCCN guidelines state that no additional surgery is required if the polyp was completely removed and has favorable histologic features. However, in patients with sessile polyps, the guidelines suggest that colectomy is an option because sessile polyps are associated with a greater incidence of adverse outcomes.
Patients who present with invasive colon cancers appropriate for resection should receive a complete staging workup, including biopsy, pathologic tissue review, total colonoscopy, complete blood count and chemistry profile, a carcinoembryonic antigen (CEA) determination, and baseline CT or MRI scans of the chest, abdomen, and pelvis. If the cancer is locally unresectable or the patient is medically inoperable, systemic therapy or chemoradiation is recommended, which can sometimes convert a tumor to a resectable state.
NCCN Treatment Standards for Stage I and II CRC (Version 2.2020 – March 3, 2020)
Patients with Stage I disease do not require adjuvant therapy.
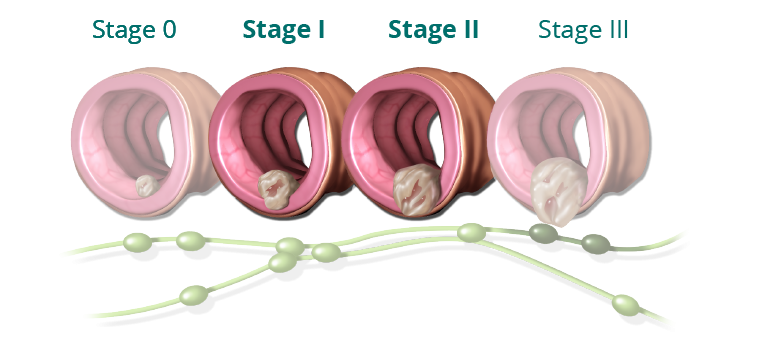
Patients with MSI-high, low-risk Stage II disease generally do not require adjuvant therapy. Other patients with low-risk Stage II disease can be observed without adjuvant therapy, or be considered for treatment with capecitabine or 5-FU/leucovorin. The NCCN panel does not consider FOLFOX therapy (which includes oxaliplatin) to be appropriate for these patients due to the long-term risks of oxaliplatin therapy. Patients with high-risk Stage II disease can be considered for adjuvant therapy with 5-FU/LV, capecitabine, FOLFOX, CAPEOX, or in some cases, observation.
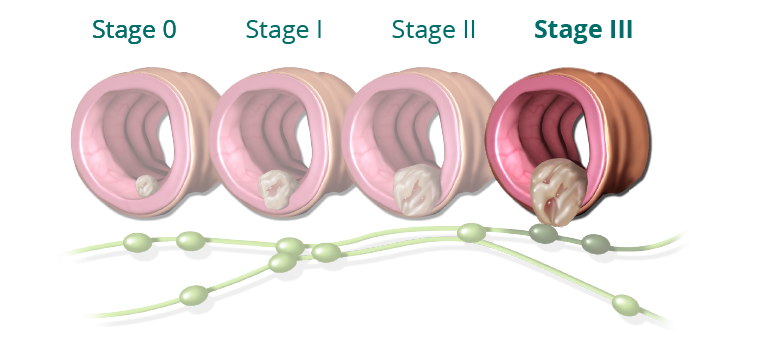
NCCN Treatment Standards for Stage III CRC (Version 2.2020 – March 3, 2020)
For patients with low-risk Stage III disease, the preferred adjuvant treatment options are 3 months of CAPEOX or 3 to 6 months of FOLFOX. In patients who should not receive oxaliplatin, other treatment options include single-agent capecitabine or 5-FU/LV. For patients with high-risk Stage III disease, the preferred adjuvant treatment options are 6 months of FOLFOX or 3 to 6 months of CAPEOX. Again, when oxaliplatin treatment is not appropriate, patients may receive single-agent capecitabine or 5-FU/LV.