WHY SOME SPECIALISTS MAY BE FRUSTRATED BY NTM
Although most pulmonologists and infectious disease specialists may feel knowledgeable about NTM and comfortable treating it first line, it can still be a frustrating disease to manage for a number of reasons. First, NTM can be very difficult to diagnose, with the diagnosis process often taking up to 2 years. Once the disease is diagnosed, treatment is burdensome for both patients and HCPs. Finally, many specialists perceive the chance of eradicating NTM in a given patient to be rather low. Recognizing the challenges of managing NTM will help you understand why HCPs choose different treatment approaches for their NTM patients.
Challenging Diagnosis
NTM can be a challenging disease to diagnose for a handful of reasons. The graph below lists the most commonly cited challenges specialists face when diagnosing NTM.
Select each issue listed below to see the percentage of HCPs who cited that issue as a challenge in diagnosing NTM:
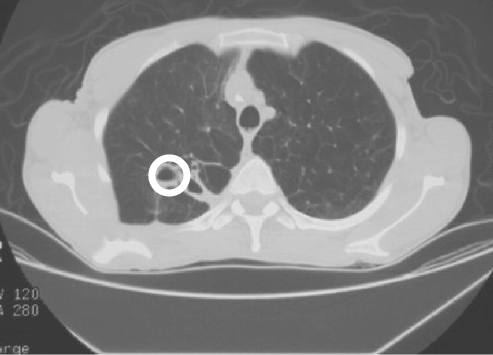
In diagnosing NTM, 82% of HCPs perform a sputum culture as soon as NTM is suspected. However, a sputum culture does not provide a definitive diagnosis: a positive Mycobacterium avium complex (MAC) culture may be due to colonization rather than infection. Remember that a colonization refers to the harmless growth of bacteria at a particular body site, whereas an infection is a growth of bacteria that causes the body harm. HCPs must also rely on clinical, microbiologic, and radiographic findings to make a diagnosis, and these can be non-specific to NTM as well.
Symptoms of NTM are not necessarily specific to NTM, which makes for a difficult diagnosis for HCPs. In addition, PCPs, who may be less knowledgeable about the disease, may not recognize the symptoms and risk factors for NTM and may not refer patients to a PUD or ID specialist for diagnosis. Complaints of coughing, wheezing, and chest pain may indicate any number of lung diseases. Similarly, radiographic findings may not be specific enough to suspect NTM, which can add to the confusion.
See what specialists have to say about the difficulty of diagnosing NTM:
Select the arrows to see quotes from physicians about NTM diagnosis.

“When it comes to symptoms, the lungs are pretty stupid. There are only so many symptoms – shortness of breath, you can cough with or without sputum, maybe have some chest pain/fluid collection, cough up blood, and wheezing. What else can you really complain of? In terms of comparing the symptoms that patients can complain of, it’s the same as everything else. What questions do you ask? What imaging do you ask for?” – PUD, Southern California

“A lot of times these NTM cases end up being referred to me by PCPs. Most patients are limited by who they can see. They’re not just waking up and deciding, ‘Oh, I think I need to see a pulmonologist or an ID doc.’ Very seldom do you see someone just show up by themselves. Once a PCP sees something in the lungs from the x-ray, that’s when they’ll refer over to the experts.” – ID, Northern California

“It’s not on [PCPs’] radar. They don’t know when or how to treat or whether someone has the disease. But they understand MAC is a potential pathogen.” – ID, New York

“Sometimes [patients] get referred to me, and sometimes they’ll seek out a specialist on their own, because people have been saying it’s asthma, but nothing’s working, so they seek out a specialist. It’s very possible that patients have had [NTM] a long time before they come to me.” – PUD, Pennsylvania

“PUDs do procedures to rule out other diseases. So with NTM, most of the time patients will come to me with a chronic cough or maybe an abnormal CT finding, so going down the diagnostic algorithm of pulmonary nodules and bronchiectasis and ruling out other potential diseases or other connective tissue diseases, like rheumatoid arthritis for instance, that might be putting the patient at risk or causes the problem in the first place.” – PUD, Southern California
Previous
Next
Burdensome Treatment
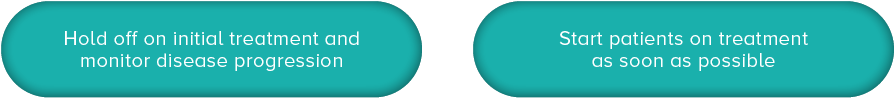
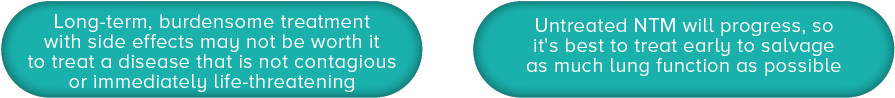
NTM treatment can be burdensome for both patients and HCPs; learning why NTM treatment can be so difficult will help you understand the rationale of some HCPs who have chosen not to treat some of their NTM patients and instead “wait and watch.”
First, the side effects of guidelines-based therapy (GBT) for NTM patients can be challenging. Below is a list of common side effects of GBT and the impact they have on patients’ quality of life.
Select each button to reveal common side effects of GBT and the impact they have on patients’ quality of life.
In addition to being difficult to tolerate, NTM therapy is lengthy. It can take up to 18 months, including achievement of culture conversion, which may take up to 6 months, and an additional 12 months of continuing therapy after culture conversion. NTM therapy may also require multiple treatment courses if disease recurs. ATS/IDSA-recommended treatment consists of at least 3 recommended medications, and patients need to visit the doctor’s office frequently for ongoing monitoring and treatment follow-up. As a result, the decision about when to initiate therapy and the choice of treatment regimen depend largely on the goals for each specific patient, disease severity, and patient comorbidities.
Perceived Low Chance of Permanent Eradication
In some specialists’ experience, NTM has a high probability of relapse and/or reinfection. This may explain why HCP satisfaction with current treatment options is not particularly high, with only 27% of HCPs saying they are very satisfied with GBT.
Consider the following example to understand why many HCPs may feel that NTM is difficult to treat and that GBT is a challenging treatment option for their NTM patients. Keep in mind that the HCPs included in the research below were selected because they are actively managing NTM patients.
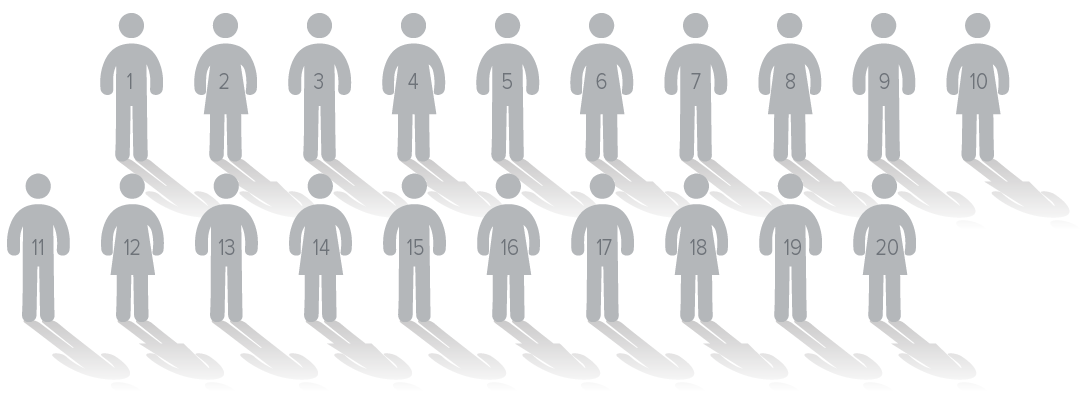
The average PUD/ID sees approximately 20 NTM patients in 3 years. Select the buttons below to learn more about these NTM patients.

Approximately 63% of NTM patients have successful treatment, leaving another 37%, or about 8 patients for each specialist, still struggling with NTM

On average, another 28%, or about 3 of each specialist's patients, who had successful treatment will either relapse or be reinfected with NTM.
This means every PUD/ID will have, on average, 11 NTM patients over the course of 3 years who need better treatment options than what is currently available for NTM.