What was the stage of Pedro’s diseaseat initial diagnosis?
Pedro’s cancer was confined to the prostate, had not spread to the lymph nodes, and wasnonmetastatic (stage T2N0M0)
Pedro is a 71-year-old Hispanic man who was noted to have dysuria in July 2017. A concomitant workup was obtained, revealing a prostate-specific antigen (PSA) level of 10.7 ng/mL. His urine culture was negative for pathogens. He was thought to have a urinary tract infection and was treated by his primary care physician with antibiotic therapy for 7 days. The dysuria resolved rapidly, but a follow-up PSA done 2 weeks later was still elevated at 11.1 ng/mL. The patient was then referred to a urologist for further evaluation. The urologist performed a digital rectal exam (DRE) and noted a small irregularity in the left lobe of an estimated 40-g prostate.

Transrectal ultrasonography confirmed a hypoechoic area in the left lobe of the prostate. A 12-core biopsy of the prostate was performed. Results showed a Gleason 7 (4+3) adenocarcinoma of the prostate in 4/12 cores. The urologist then discussed the various therapeutic options available including radical (robotic) prostatectomy, radiation therapy, and other local modalities including high-intensity focused ultrasound (HIFU). Total body bone scan and computed tomography (CT) scan of the abdomen and pelvis did not reveal any bone, liver, or nodal metastases.
As the patient had some significant prior medical problems, he wanted to see the radiation oncologist. He ultimately opted for low-dose rate (LDR) brachytherapy, which he tolerated well. He is following up with both his radiation oncologist and urologist.
What was the pathologic stage of Phil’s diseaseat initial diagnosis?
Phil’s cancer was confined to the prostate and his nearby lymph nodes were not assessed (stage T2Nx)
Phil is a very healthy 57-year-old marathon runner who had not seen a physician in years. A routine physical exam in March 2014 was normal except for a digital rectal exam that revealed a vague irregularity in the right lobe of the prostate, which was otherwise normal in size. A prostate-specific antigen (PSA) test done at that time was 6.8 ng/mL. He was referred to a urologist who confirmed the finding on physical exam.
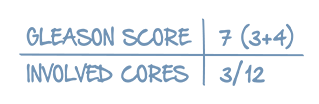
Transrectal ultrasound with color-flow doppler revealed calcifications in the right lobe of the prostate with associated hypervascularity but without a dominant mass. A 3.0 Tesla MRI revealed decreased signal intensity in the peripheral zone of the base of the right lobe of the prostate that appeared organ-confined. A subsequent biopsy revealed a Gleason 7 (3+4) adenocarcinoma of the prostate in 3/12 cores. The patient noted a history of breast cancer in his maternal aunt but no family history of prostate cancer. His parents are both alive and relatively healthy in their mid-80s.
After careful discussion with his urologist and knowing the risks and benefits of treatment, the patient decided to undergo radical (robotic) prostatectomy, which was uncomplicated. Pathology from the procedure revealed a T2Nx cancer with the same pathologic features as the biopsy and no upgrade. Follow-up PSA several weeks after the procedure was <0.1 ng/mL and has remained undetectable for the past 3 years.
What was the pathologic stage of Thanh’s diseaseat initial diagnosis?
Thanh’s cancer was confined to the prostate, had not spread to the lymph nodes, and was nonmetastatic(stage T2N0M0)
Thanh is a 72-year-old Vietnamese man who was noted by his primary care physician to have a prostate-specific antigen (PSA) level of 7.8 ng/mL in September 2012.
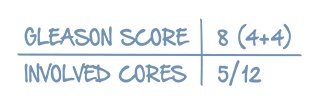
He was referred to a urologist, who performed a transrectal ultrasound-guided (TRUS) biopsy that revealed a Gleason 8 (4+4) adenocarcinoma of the prostate in 5/12 cores. In reviewing his history, the urologist noted that Thanh emigrated to the US in 1973 but was exposed to the defoliant Agent Orange for several years prior. A staging workup with a total body bone scan and a computed tomography (CT) scan of his abdomen and pelvis were unremarkable for metastases.
After discussing it with his family and the urologist, Thanh underwent radical prostatectomy, which confirmed a Gleason 8 prostate cancer. All 18 lymph nodes removed via extended pelvic lymph node dissection revealed no evidence of tumor involvement, so his pathologic stage was T2N0M0.
He followed up with his urologist 2 weeks after surgery and then every 3 months. All subsequent PSA measurements were <0.1 ng/mL until November 2014, when his PSA was 0.3 ng/mL. Follow-up PSA was done twice more over the next 3 weeks and was 0.4 ng/mL on both occasions. Thanh refused any further imaging and was referred by his urologist to a radiation oncologist who treated him with:
- Salvage intensity-modulated radiation therapy (IMRT)
- Neoadjuvant, simultaneous, and adjuvant leuprolide
He completed leuprolide therapy in November 2016. His PSA nadir was 0.2 ng/mL at the end of his treatment. He experienced significant fatigue and hot flashes with leuprolide therapy. In 2017, his PSA levels were measured at:
- 0.8 ng/mL in April
- 1.2 ng/mL in June
- 2.8 ng/mL in August
- 4.6 ng/mL in October
He is asymptomatic, and conventional imaging with total body bone scan and CT scan of the abdomen and pelvis are negative. He refused an Axumin scan but agreed to be treated with a dose of leuprolide given last month and intermittently for the near-term.
What was the pathologic stage of Stan’s diseaseat initial diagnosis?
Stan’s cancer had grown outside the prostate into the seminal vesicles and involved 1 or more lymph nodes(stage T3bN1)
Stan is a 61-year-old African American man who is a station chief in the Middle East for a government intelligence agency.
In 2013 while still in the US, Stan underwent a radical prostatectomy and extended pelvic lymph node dissection for a T3bN1 Gleason 8 prostate cancer that found 3/17 involved nodes, seminal vesicle involvement, and negative margins. He refused the recommended adjuvant radiation or androgen deprivation therapy (ADT). His postoperative course and initial follow-up were uncomplicated.
Records from his urologist between 2013 and 2014 were reviewed and showed that all postoperative prostate-specific antigen (PSA) levels were <0.1 ng/mL. He took on his new assignment in the Middle East in early 2015 and promised to follow up with physicians at a prestigious academic medical center in Amman, Jordan. After 2 visits, his PSA remained undetectable but work demands precluded regular follow-up for the ensuing 2 years.
By the time he returned for follow-up, his PSA had risen to 3.4 ng/mL. He was asymptomatic and bone and computed tomography (CT) scans were negative for metastases. He was offered salvage radiotherapy but declined it as he felt that he was unlikely to be cured. His PSA values each month for the next 3 months were:
- 4.9 ng/mL
- 5.8 ng/mL
- 6.9 ng/mL
This put his PSA doubling time (PSADT) at approximately 3 months. He requested transfer back to the US and saw his previous urologist, who had performed the original prostatectomy. After another test showed a PSA of 7.5 ng/mL and he had an extensive discussion of risks and benefits with his health care providers, he agreed to be treated with a single dose of leuprolide 22.5 mg.
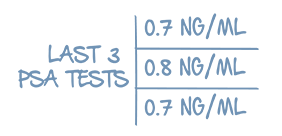
His last several PSA levels have been 0.7 ng/mL, 0.8 ng/mL, and 0.7 ng/mL, respectively, each month for the last 3 months. He remains clinically stable with no symptoms. There has been no discussion of continuing any treatment.
What was the stage of Sam’s diseaseat initial diagnosis?
Sam’s cancer had grown into the tissues next to the prostate (the right ilium), his nearby lymph nodes were not assessed, and the cancer had spread to distant lymph nodes (stage T4NxM1a)
Sam is a 92-year-old veteran who experienced multiple gunshot wounds and shrapnel injuries and was honorably discharged. Over the next several decades, his main medical problem was chronic pain syndrome requiring a variety of analgesics including opioids. In 2017, his pain became disproportionately localized to his pelvis, making ambulation difficult. He also reported having blood in his urine.
He saw his pain medicine specialist who ordered x-rays of the pelvis, which demonstrated nearly complete replacement of the right ilium by sclerosis. Sam was referred for interventional radiology where he underwent percutaneous biopsy of the affected area. The pathology result demonstrated a poorly differentiated carcinoma that required special stains. The result was positive for cytokeratin and prostate-specific antigen (PSA) consistent with an epithelial carcinoma likely of prostatic origin. Sam was then seen by a urologist who felt a large, hard, fixed mass in the prostatic fossa. The urologist completed the workup including a total body bone scan that confirmed the right pelvic abnormality and showed several areas of uptake in the ribs and sternum consistent with chronic injury. A computed tomography (CT) scan of the abdomen and pelvis showed a 7.5 cm mass replacing the entire prostate and extending to the right ilium, with local invasion associated with a mild right hydronephrosis and bilateral retroperitoneal lymphadenopathy. PSA was drawn and was 755 ng/mL. The patient’s case was presented at Tumor Board where his stage was T4NxM1a and recommendations for palliative radiotherapy to the right ilium along with leuprolide were made and offered to the patient and his caregivers. He was not thought to be a candidate for docetaxel.
Sam had a living will but agreed with the treatment recommendations. He had prompt improvement in his pain and within 1 month his PSA levels had dropped to 80 ng/mL. He stayed on monthly leuprolide after completing his radiotherapy, and subsequent PSAs were 35 ng/mL, 15 ng/mL, and 9.4 ng/mL, respectively. He is following up with radiation oncology and his pain syndrome is back to a baseline level.
What was the stage of David’s disease at initial diagnosis?
David’s cancer appeared to be confined to the prostate, had spread to nearby lymph nodes, and had spread to other organs including the liver and lung (stage T2N1M1c)
David is a 58-year-old white man and amateur golfer who experienced a twinge of back pain while playing golf followed by easy bruising and hematuria later that day. He was seen at an urgent care clinic where he was noted to have severe thrombocytopenia with a platelet count of 10,000/μL. He was referred emergently to the hospital where the hematologist diagnosed him with a primary fibrinolytic syndrome (abnormal activation of the clot-busting pathway leading to low platelets, depletion of clotting factors, and elevation of fibrin split products).
X-rays of the thoracic spine revealed compression fractures of the T4–T9 vertebrae. A bone scan showed widespread metastatic disease involving multiple vertebrae, ribs, and pelvis. A computed tomography (CT) scan of the chest, abdomen, and pelvis showed suspicious 2.0 cm lesions in the liver and lung. Magnetic resonance imaging (MRI) of the brain with gadolinium was negative for metastases and a biopsy of a rib lesion demonstrated a high-grade carcinoma. Digital rectal exam was positive for a hard mass involving the right lobe of the prostate. His prostate-specific antigen (PSA) level was 325 ng/mL.
After aggressive transfusion of platelets, fresh frozen plasma, and cryoprecipitate, David was administered degarelix (Firmagon®) and docetaxel chemotherapy starting that evening. His bleeding subsided quickly. His pain improved over the next few weeks and he resumed playing golf 6 weeks after his initial presentation. He completed 6 cycles of docetaxel chemotherapy and was switched over to every-3-month injections of leuprolide.
His PSA after 6 months was 1.8 ng/mL and he was asymptomatic except for some nail changes, alopecia, and fatigue from the docetaxel, and loss of libido and hot sweats attributable to leuprolide. He is awaiting the results of his latest CT and MRI scans.
What was the pathologic stage of Chris’s disease at diagnosis at initial diagnosis?
Chris’s cancer was confined to the prostate, had not spread to the lymph nodes, and was nonmetastatic(stage T2N0M0)
Chris is a 63-year-old white man currently in long-term incarceration. He was treated in the prison system for a T2N0M0 Gleason 7 prostate cancer with radical intensity-modulated radiation therapy (IMRT) to the prostatic bed and neoadjuvant leuprolide followed by 6 months of adjuvant leuprolide. His prostate-specific antigen (PSA) level at the time of his diagnosis was 11.3 ng/mL and dropped over 2 years to a nadir of 1.5 ng/mL. His follow-up was intermittent; he’s just been referred to prison medical locally due to complaints of pain in his lower back and right femur. The correctional officers denied him access to medical care until he started to develop shortness of breath.
In the infirmary, he was in significant pain and needed oxygen. He was referred immediately to the hospital where his workup revealed the following:
- X-ray of right femur positive for a displaced pathologic fracture and extensive replacement by sclerotic tumor
- Total body bone scan positive for a “superscan” with intense tracer uptake in numerous areas of the axial and extra-axial skeleton
- Computed tomography (CT) scan of chest, abdomen, and pelvis positive for bilateral pulmonary emboli, retroperitoneal adenopathy, and an extensive right iliofemoral deep venous thrombosis (DVT)
- PSA 412 ng/mL
Chris was admitted into the intensive care unit (ICU) and stabilized. He was placed on intravenous heparin for the DVT and patient-controlled analgesia (PCA) for the severe pain, and then taken to the operating room for an open reduction and internal fixation of the right femur, which was uncomplicated. He began to stabilize and was seen in consultation by a radiation oncologist who offered Chris a course of palliative external beam radiation therapy (EBRT) to the right femur. A medical oncologist then saw Chris after he moved out of the ICU and offered him degarelix (Firmagon®) immediately followed by docetaxel. Once stable, Chris was discharged on warfarin with instructions to the penitentiary to follow up weekly for blood counts and international normalized ratio (INR) monitoring. Chris eventually completed 6 cycles of docetaxel and switched over to every-3-months leuprolide, which he remains on today. His PSA declined but after 6 months was still hovering around 20 ng/mL.
What was the pathologic stage of Don’s diseaseat initial diagnosis?
Don’s cancer was confined to the prostate, had spread to 4 nearby lymph nodes, and was nonmetastatic(stage T2N1M0)
Don is a 70-year-old retiree who maintains a healthy lifestyle. He presented with a localized Gleason 9 (5+4) prostate carcinoma in 5/12 cores in 2009. His prostate-specific antigen (PSA) at the time was 12.6 ng/mL. He underwent radical prostatectomy and pelvic lymph node dissection 2 weeks later.
- 4/8 nodes positive
- Postsurgical PSA <0.1 ng/mL
- T2N1M0
He agreed to a 2-year course of adjuvant leuprolide administered at the urologist’s office every 3 months but refused adjuvant radiation. He was not seen by a urologist for 3 years until a PSA test performed earlier this year measured 47.5 ng/mL.
His urologist ordered a bone scan and a computed tomography (CT) scan of the chest, abdomen, and pelvis. The bone scan revealed a total of 4 lesions in the thoracic and lumbar spine and an isolated metastasis in the left humerus. The CT scans were unremarkable. He was referred to a medical oncologist.
Don and his family opted for docetaxel along with leuprolide, citing the 4.5 months of docetaxel therapy as their reason. He completed all 6 cycles of docetaxel and remains on leuprolide every 3 months. His PSA is 0.9 ng/mL and he is asymptomatic. He continues to follow up with his oncologist.
What was the clinical stage of John’s diseaseat initial diagnosis?
John’s cancer was confined to the prostate, had spread to 3 lymph nodes, and he was not assessed for metastatic disease (stage T3N1M0)
John was an 84-year-old white man who was diagnosed with a Gleason 9 (5+4) adenocarcinoma of the prostate in 2008 (11/12 cores involved, prostate-specific antigen [PSA] 17 ng/mL). A staging workup revealed that the tumor involved the seminal vesicle, extended beyond the prostatic capsule, and approached but did not involve the inferior surface of the bladder. He had 3/8 lymph nodes positive but no evidence of bone, lung, or liver metastases. His clinical stage was T3N1M0. He was asymptomatic, was not a candidate for surgery or radiation therapy, and elected to be followed by his urologist without any specific treatment.
In 2010, approximately 2 years after he was diagnosed, his PSA was found to be 58 ng/mL and he began to develop urinary frequency. Scans were repeated but still showed no evidence of metastases. After careful discussion with his urologist, John started treatment with leuprolide 7.5 mg intramuscular (IM) and then 22.5 mg IM every 3 months. His PSA quickly reached a nadir of 1.8 ng/mL after 4 months. His urinary frequency resolved and he had no pain. For the next 2.5 years:
- PSA ranged between 1.8 ng/mL and 2.5 ng/mL
- His testosterone levels were consistently <50 ng/dL
In 2012, his PSA began to rise with a doubling time of 3 months and peaked at 15.8 ng/mL, at which point his urologist placed him on bicalutamide 50 mg by mouth daily and continued the leuprolide on the same schedule of every 3 months. This regimen kept John’s PSA under 5 ng/mL for approximately 9 months, but in mid-2014, John’s PSA climbed to 10.4 ng/mL and 14 ng/mL within 2 weeks of each other. His urologist discontinued the bicalutamide and followed him monthly. Within 2 months, his PSA was 26.7 ng/mL. A total body bone scan was conducted and was positive for multiple vertebral and pelvic metastases.
His urologist added abiraterone acetate (Zytiga®) plus prednisone for approximately 10 months until July 2015, when a CT scan showed several 1.0 cm liver metastases. He was taken off abiraterone acetate but kept on prednisone to help with bone discomfort. He refused chemotherapy and was treated by palliative care specialists until his death in June 2016.
What was the pathologic stage of Antonio’s diseaseat initial diagnosis?
Antonio's cancer had grown outside of the prostate, had not spread to the lymph nodes, and was nonmetastatic(stage T3N0M0)
Antonio is a 70-year-old Filipino man. He was diagnosed with a Gleason 8 (4+4) prostate cancer in 2007 and underwent a radical prostatectomy with extended pelvic lymph node dissection. His prostate-specific antigen (PSA) prior to surgery was 14.3 ng/mL; postoperatively, it dropped to <0.1 ng/mL. His final pathologic stage was T3N0M0. In 2012, his PSA was undetectable, then rose to 0.4 ng/mL. His doctor chose to monitor him closely and saw his PSA rise rapidly over 2 to 3 weeks:
- Undetectable
- 0.4 ng/mL
- 0.6 ng/mL
- 0.7 ng/mL
His bone and CT scans were unremarkable. He underwent salvage pelvic radiotherapy followed by 2 years of adjuvant leuprolide. His testosterone levels were <50 ng/dL for the entire treatment period and his PSA remained at 0.2 ng/dL. He completed all treatments in August 2014. Over the next year, his testosterone levels rose sluggishly until peaking at 125 ng/dL. In December 2015, his PSA rose again to 0.5 ng/dL. His radiation oncologist started him back on continuous leuprolide.
Despite treatment, his PSA continued to rise to 1.2 ng/mL, 2.3 ng/mL, and 3.7 ng/mL, respectively, when checked monthly (PSA doubling time <2 months). A total body bone scan was performed and showed 2 questionable foci of bony involvement in the left pubic ramus and the C5 vertebra. The results were possibly attributable to degenerative change. His medical oncologist added bicalutamide 50 mg but discontinued it after his liver enzymes were elevated. Although Antonio achieved some PSA response, he also had nausea and vomiting (controlled with antiemetics). His PSA rose in July 2016 to 6.6 ng/dL. His testosterone level was 17 ng/dL. A bone scan confirmed progression of the lesions in the pubis and C5 vertebrae along with a new lesion in the right fourth rib. He agreed to a course of 3 infusions of sipuleucel-T (Provenge®) administered every 2 weeks for 3 infusions. His PSA remained steady. His oncologist then treated him with enzalutamide (Xtandi®) as Antonio wanted to limit medical visits and monitoring. He refused denosumab (Prolia®). His PSA went down to 4.2 ng/mL but six months later in February 2017, he experienced PSA progression and had 2 new thoracic spine lesions. A follow-up bone scan at 6 months showed progression in bone lesions. Antonio began radium-223 infusions. His first infusion was well tolerated. Currently, his PSA is 4.7 ng/dL but his pain has improved. He is still working and is looking forward to his next infusion later this month.
What was the stage of Prem’s disease at initial diagnosis?
Prem’s cancer was confined to the prostate, had not spread to the lymph nodes, and was nonmetastatic(stage T2N0M0)
Prem is a 72-year-old Indian man and retired engineer. He was diagnosed with a Gleason 8 prostate cancer in 2010:
- Prostate-specific antigen (PSA) 4.9 ng/mL
- Stage T2N0M0
- Bone and CT scans unremarkable
Prem was treated with 81.0 Gy of intensity-modulated radiation therapy (IMRT) that was tolerated well but noteworthy for chronic mild diarrhea that eventually resolved after 2 years. His PSA nadir was 0.8 ng/mL and remained stable until mid-2013. At that point, his PSA rose, with a PSA doubling time (PSADT) of 10.4 months. His bone and CT scans remained normal.
In the latter part of 2014, his PSA increased rapidly to 5.2 ng/mL. Prem always came to his visits with a spreadsheet, and noted the increase not only in PSA but in slope. The PSADT was recalculated at 8 months. He pointed this out to the urologist, who offered him intermittent androgen deprivation therapy (ADT). His PSA responded initially, but eventually crept up over 10 ng/mL in early 2017 despite continuous ADT. His testosterone was checked and was 12 ng/dL. His bone and CT scans remained negative. Prem insisted on a second drug and “wanted everything done.” The urologist added bicalutamide 50 mg by mouth daily, and Prem remains on that treatment today. His PSA has responded, and is currently 3.7 ng/mL. Prem remains active and asymptomatic and has been following up with his urologist every 3 months.
What was the pathologic stage of Al’s diseaseat initial diagnosis?
Al's cancer had grown outside the prostate, had not spread to the lymph nodes, and was nonmetastatic(stage T3N0M0)
Al is a 49-year-old retired football player who suffers some of the chronic neurological effects of that sport (eg, short-term memory loss, emotional lability). He was diagnosed with prostate cancer in 2010 (prostate-specific antigen [PSA] 7.4 ng/mL, T3N0M0, Gleason 9). He underwent radical prostatectomy and recovered well. Al had prolonged impotence, which worsened his depression. His PSA in follow-up never went to an undetectable level, and the nadir was 0.5 ng/mL measured 3 months later. His wife asked the urologist if “something else could be done.” She brought up Al’s history of prostate and breast cancer in multiple close relatives, all of whom were diagnosed at similarly early ages. Al was referred to a genetic counselor who confirmed that he was positive for BRCA mutation. The urologist reviewed the pathology result and thought that there may have been a tumor as close as 1 mm from the inked surgical margin. The urologist then referred Al to a radiation oncologist who administered adjuvant radiation therapy along with neoadjuvant, concurrent, and adjuvant leuprolide for a total of 2 years. At that point, Al became permanently impotent and developed some urinary incontinence. All treatment concluded in the latter part of 2012. His nadir PSA at that point was 0.3 ng/mL.
In early 2014, Al’s PSA rose. His PSA doubling time (PSADT) was 1.6 months. Continuous leuprolide was started immediately and his PSA declined to 2.2 ng/mL, which was maintained for approximately 18 months. MRI and computed tomography (CT) scans showed no signs of metastatic disease. His PSA rose again to 5.3 ng/mL in early 2016 and ketoconazole was added initially at 200 mg by mouth three times daily and then 400 mg three times daily. His serum testosterone levels varied between 20 ng/dL and 30 ng/dL on several occasions while he was taking leuprolide. His bone and CT scans still showed no evidence of metastatic disease. Al remained on ketoconazole until mid-2017, when his PSA climbed again to 8.8 ng/mL. His bone and CT scans were still negative in July 2017. Al and his wife are anxious to begin a new therapy but are concerned by his mood swings, his worsening cognitive dysfunction, and the overall pace of his disease.